Clinical Practice Guidelines for Management of Neonates at Risk or Suspected of Early-Onset Neonatal Sepsis (EONS)
- Mayta
- Aug 13, 2024
- 5 min read
Objective:
Early-onset neonatal sepsis (EONS) is a significant cause of mortality and both short-term and long-term complications in newborns. This guideline aims to provide a comprehensive framework for screening, managing, and treating newborns at risk for or suspected of having EONS.
Definition:
Neonates at risk for EONS include those with any of the following:
Premature rupture of membranes (PROM) for ≥18 hours (prolonged PROM)
Positive maternal group B streptococcus (GBS) rectovaginal culture at ≥35 weeks gestation
Suspected or confirmed maternal intrauterine inflammation and/or infection (triple I)
Indication for intrapartum antibiotic prophylaxis (IAP) for GBS but not received or received inadequately
Preterm birth <37 weeks gestation without known etiology (excluding indicated preterm birth due to maternal factors such as severe pre-eclampsia, antepartum hemorrhage, etc., without PROM)
Diagnosis of Intrauterine Inflammation and/or Infection (Triple I):
Diagnosis of placental and amniotic fluid infection is based on the following criteria:
Table 1: Diagnostic Criteria for Maternal Fever and Placental/Amniotic Fluid Infection
Condition | Diagnostic Criteria |
Isolated Maternal Fever | - Oral temperature ≥39°C or - Oral temperature 38.0–39.0°C with repeat measurement ≥38.0°C within 30 minutes |
Suspected Triple I | Maternal fever of unknown origin plus one of the following: - Fetal tachycardia >160 bpm for ≥10 minutes, excluding accelerations, decelerations, and periods of fetal heart rate variability - Maternal WBC count >15,000/mm³ without steroid use - Purulent fluid from the cervical os |
Confirmed Triple I | Criteria for suspected triple I plus one of the following: - Positive Gram stain of amniotic fluid obtained by amniocentesis - Positive amniotic fluid culture or low amniotic fluid glucose |
Intrapartum Antibiotic Prophylaxis (IAP):
Indications for IAP:
History of previous infant with invasive GBS disease (e.g., sepsis, meningitis)
GBS bacteriuria during current pregnancy (any trimester)
Positive GBS rectovaginal culture during the current pregnancy
Unknown GBS carrier status or GBS culture, and any of the following: a. Preterm birth <37 weeks gestation b. PROM ≥18 hours c. Intrapartum fever (oral temperature ≥38°C)
IAP Not Indicated:
History of GBS colonization in previous pregnancies (unless indicated in the current pregnancy)
History of GBS bacteriuria in previous pregnancies (unless indicated in the current pregnancy)
Cesarean delivery before labor onset and with intact membranes
Adequate IAP:
Penicillin, ampicillin, or cefazolin administered for ≥4 hours before delivery
Inadequate IAP:
No IAP despite indication
Antibiotics other than penicillin, ampicillin, or cefazolin
Antibiotic duration <4 hours before delivery
Sepsis Screen:
The initial laboratory evaluation for neonates at risk for or suspected of EONS includes:
Complete blood count (CBC) with differential count
Peripheral blood smear
Acute phase reactants: micro ESR (mESR) or C-reactive protein (CRP)
Sepsis Screen Interpretation:
Positive Screen:
Abnormal absolute neutrophil count (ANC) for gestational age and postnatal age: <5th percentile or >95th percentile
Immature: total neutrophil ratio (I/T ratio) >0.2
Abnormal acute phase reactants: a. mESR: - Birth–72 hours: >10 mm/hr - >72 hours: >15 mm/hr b. CRP >10 mg/L
Management of Neonates at Risk for EONS:
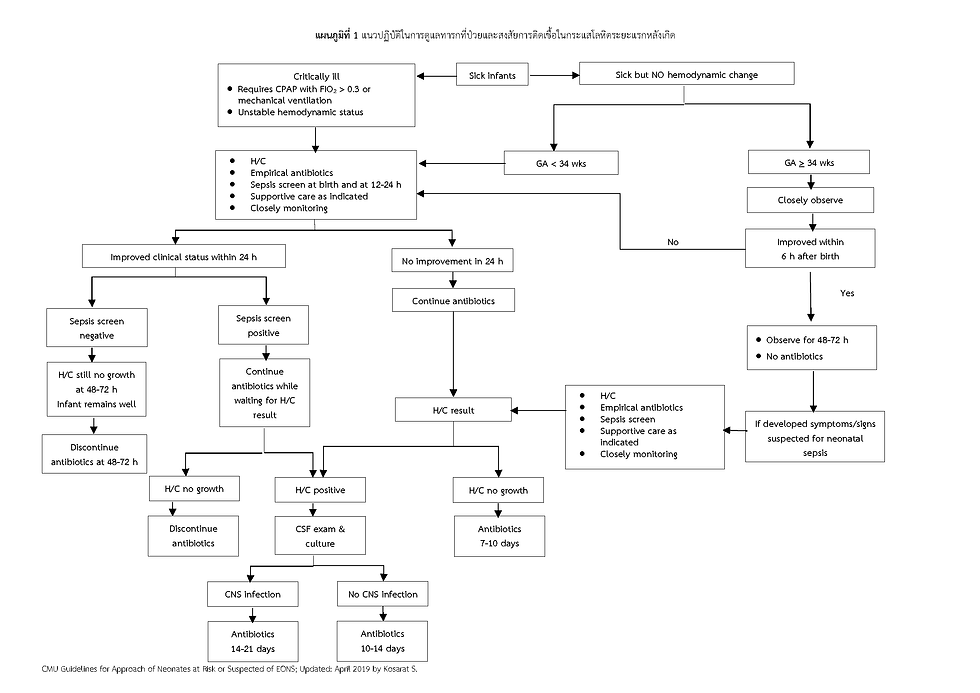
1. Ill neonates: This includes neonates with signs or symptoms suggestive of infection such as respiratory distress, temperature instability, hypotension, and cyanosis. They are categorized into two groups:
a. Critically ill neonates: This includes neonates requiring CPAP with FiO2 >0.3 or mechanical ventilation, those with hypotension, or shock. The initial management should include:
Blood culture (or hemoculture) and immediate empirical antibiotic therapy
Sepsis screen at birth and 12-24 hours
Supportive care as indicated (e.g., respiratory support, blood pressure management, fluid and electrolyte management, glucose management, and temperature regulation)
Close monitoring of vital signs, physical examination, and clinical status
b. Sick but not critically ill neonates: This includes neonates with signs of illness within the first 6 hours of life such as respiratory distress and cyanosis but without critical illness. Management should be based on gestational age:
Gestational age <34 weeks: Manage as critically ill neonates.
Gestational age ≥34 weeks:
Close observation with vital signs every hour for 4 hours, then every 4 hours for at least 24-48 hours.
Supportive care as indicated.
If clinical improvement within 6 hours after birth:
No antibiotics or further laboratory investigations are needed.
Continue close observation for signs of deterioration.
If no improvement within 6 hours or clinical deterioration:
Obtain sepsis screen, blood culture, and start empirical antibiotics.
Manage according to the results of sepsis screen and blood culture as described for critically ill neonates.
2. Asymptomatic neonates: This includes neonates with risk factors for EONS but without any signs or symptoms. Management is based on the presence or absence of maternal history of suspected or confirmed triple I:
a. Suspected or confirmed maternal triple I:
- Immediate blood culture
- Empirical antibiotics
- Sepsis screen at 12-24 hours
- Close observation for signs of deterioration
b. No maternal history of suspected or confirmed triple I: - Gestational age <34 weeks:
Blood culture and sepsis screen at 12-24 hours
Consider empirical antibiotics after blood culture.
Close observation for signs of deterioration.
- Gestational age ≥34 weeks:
Sepsis screen at 12-24 hours.
Close observation.
If the sepsis screen is negative and the infant remains asymptomatic, no antibiotics are needed, but continue observation in the hospital for 48-72 hours.
If the sepsis screen is positive:
Obtain blood culture.
Start empirical antibiotics.
Close observation.
Manage according to blood culture results as described for other groups.
Antibiotic Selection in Neonates with Suspected or Proven EONS:
Selection should be based on the local epidemiology of pathogens.
Ampicillin and Gentamicin are the preferred first-line antibiotics.
Ampicillin (Dosage: 50 mg/kg/dose every 12 hours IV for neonates <7 days old, and every 8 hours for neonates ≥7 days old).
Gentamicin (Dosage: 5 mg/kg/dose IV every 24 hours).
The most common pathogens in EONS are GBS, E. coli, Listeria monocytogenes, and other gram-negative bacteria.
The recommended initial empirical antibiotics are penicillin or ampicillin plus an aminoglycoside.
Cefotaxime (a third-generation cephalosporin) is not recommended for routine empirical treatment due to the risk of rapid emergence of resistance. However, it has good cerebrospinal fluid penetration and can be considered for meningitis treatment or in neonates with contraindications to aminoglycosides.
Ceftriaxone is not recommended in neonates due to its high albumin-binding affinity, which can displace bilirubin from albumin, increasing the risk of bilirubin encephalopathy in neonates with hyperbilirubinemia.
Duration of Antibiotic Therapy:
Bacteremia without a focus:
10 days for GBS or other gram-positive bacteria.
10-14 days for gram-negative bacteria.
Meningitis:
GBS: 14 days without complications. A repeat lumbar puncture is recommended at 24-48 hours after starting antibiotics. If the cerebrospinal fluid is still abnormal, investigate for complications.
Gram-negative bacteria: At least 21 days or 14 days after a negative cerebrospinal fluid culture, whichever is longer.
Localized GBS infection:
Osteomyelitis or septic arthritis: 3-4 weeks
Endocarditis or ventriculitis: At least 4 weeks
Discontinue antibiotics within 48 hours if infection is ruled out. Prolonged broad-spectrum antibiotic use for >5 days in preterm infants is associated with an increased risk of necrotizing enterocolitis (NEC) and mortality.
References:
Faculty of Medicine, Chiang Mai University, 2019.





Commenti